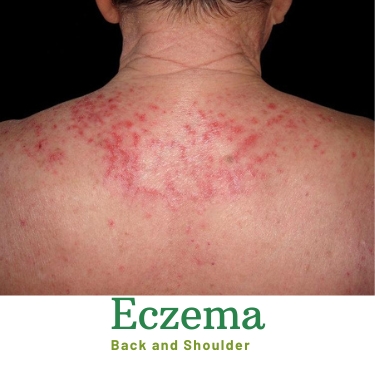
Eczema, or atopic dermatitis, is a chronic skin condition characterized by inflammation, itchiness, and rash formation. While its exact cause remains elusive, researchers have long suspected a connection between eczema and immune system function. Understanding the intricate relationship between eczema and the immune system is crucial for developing effective treatments and improving patient outcomes.
What is the Immune System?
The immune system is the body’s defense mechanism against harmful pathogens, toxins, and other foreign invaders. It comprises a complex network of cells, tissues, and organs working together to identify and neutralize threats to the body’s well-being.
How Does the Immune System Work?
When the immune system detects a foreign substance, such as bacteria or viruses, it triggers a response to eliminate the threat. This response involves various types of immune cells, including white blood cells, antibodies, and cytokines, working in concert to mount a defense and restore balance to the body.
Eczema and Immune System Interaction
In individuals with eczema, the immune system is often in a heightened activation state, leading to chronic inflammation and skin barrier dysfunction. Genetic predisposition, environmental factors, and immune dysregulation all contribute to developing and exacerbating atopic dermatitis symptoms.
The Role of the Immune System in Eczema Development
Research suggests that defects in the skin barrier, coupled with immune system abnormalities, play a central role in atopic dermatitis pathogenesis. Dysfunctional immune responses, such as exaggerated inflammatory reactions, can trigger flare-ups and perpetuate the cycle of skin irritation and inflammation.
Factors Influencing the Immune System in Eczema
Several factors influence immune system function in eczema, including genetics, allergen exposure, microbial imbalance, and environmental triggers. Understanding these factors is essential for devising personalized treatment approaches tailored to each individual’s needs.
Impact of Immune Dysfunction on Eczema Severity
Immune dysfunction contributes to the development of eczema and influences its severity and treatment response. Patients with compromised immune function may experience more frequent and severe flare-ups, challenging symptom management.
Relationship between Immune Dysfunction and Eczema Flare-ups
Studies have shown that alterations in immune cell function and cytokine production contribute to the inflammatory cascade observed in eczema. Dysregulated immune responses can lead to persistent itching, redness, and skin lesions characteristic of eczema flare-ups.
How Immune Dysregulation Affects Eczema Treatment Outcomes
Immune dysregulation can also impact the efficacy of eczema treatments, such as topical corticosteroids, immunomodulators, and biologic agents. Individuals with underlying immune deficiencies may require tailored treatment strategies for optimal symptom control and disease management.
Managing Eczema Through Immune System Support
Addressing immune dysfunction is critical to managing eczema and improving patient outcomes. Several strategies aim to bolster immune function and mitigate inflammation to effectively alleviate eczema symptoms.
Strategies for Bolstering Immune Function to Alleviate Eczema Symptoms
- Dietary Modifications: A balanced diet rich in antioxidants, vitamins, and essential fatty acids can support immune health and reduce inflammation.
- Stress Management: Stress can exacerbate atopic dermatitis symptoms by triggering immune responses and hormonal changes. Practicing relaxation techniques, such as meditation and yoga, can help alleviate stress and promote skin healing.
- Supplementation: Certain supplements, such as probiotics, vitamin D, and omega-3 fatty acids, may help modulate immune function and reduce atopic dermatitis severity.
- Topical Treatments: Emollients and moisturizers help restore the skin barrier and alleviate dryness, reducing the risk of atopic dermatitis flare-ups.
Lifestyle Modifications to Support a Healthy Immune System
- Regular Exercise: Physical activity boosts immune function and reduces inflammation, contributing to overall skin health.
- Adequate Sleep: Quality sleep is essential for immune regulation and tissue repair. Establishing a consistent sleep routine can improve atopic dermatitis symptoms and promote skin rejuvenation.
- Hygiene Practices: Proper hygiene, such as gentle shampoo, cleansing, and moisturizing, helps maintain skin integrity and prevents bacterial infections that can exacerbate atopic dermatitis.
Research Advances and Future Directions
Recent advancements in immunology and dermatology have shed light on the underlying mechanisms driving atopic dermatitis and immune system dysfunction. Ongoing research efforts aim to identify novel therapeutic targets and develop innovative treatments to manage atopic dermatitis better and improve patients’ quality of life.
Current Research on the Link Between Eczema and Immune System Function
Scientists are investigating the role of specific immune cells, signaling pathways, and genetic factors in atopic dermatitis pathogenesis. Emerging technologies, such as single-cell sequencing and immunophenotyping, allow for a deeper understanding of immune system dynamics in atopic dermatitis development.
Promising Avenues for Future Therapies Targeting Immune Dysfunction in Eczema
Immunomodulatory therapies, including biologics, small molecules, and immune modulators, hold promise for treating atopic dermatitis by targeting critical immune system components. Clinical trials evaluating the safety and efficacy of these novel interventions are underway, offering hope for more effective atopic dermatitis management in the future.
Conclusion
The intricate interplay between eczema and immune system function underscores the complexity of this chronic skin condition. Healthcare providers can devise targeted treatment strategies to alleviate symptoms and improve patient’s quality of life by understanding the underlying mechanisms driving atopic dermatitis pathogenesis and immune dysregulation.